By Cory A. Roberts, M.D.
A 21-year old Hispanic male presented with a several week history of watery diarrhea. He did not have associated blood or mucus in his stool. Sexual orientation was unknown. A significant travel history was denied by the patient. Other symptoms including fever and vomiting were denied. Endoscopy revealed no gross lesions and random biopsies were acquired.
The biopsies demonstrated a vague basophilic “mat” of material on the surface of the non-ulcerated colonic mucosa (figure 1). There was no evidence of either an active or a chronic colitis. Specifically, the lamina propria was not expanded; the crypts were normal in number and architecture; no acute cryptitis or crypt abscesses were present; granulomas were absent and the subepithelial collagen table was normal. The single abnormal finding consisted of the surface basophilic “haze”. A silver based special stain (Warthin-Starry) was reviewed. This stain nicely highlighted the surface coating by spirochetes (figure 2).
The two most recognized human species of spirochetes are Serpulina pilosicoli and Brachyspira aalborgi1. Intestinal spirochetosis was first used as a diagnostic term in 19672. Spirochetes have been known to be part of the gut flora since before that time3.
In general, the spirochetes are not thought to be pathogenic. The 1967 study cited above demonstrated up to nearly 10% incidence of spirochetosis in a series of consecutive biopsies4,5. Whether or not the presence of spirochete colonization in the colon is directly causative of diarrhea that some patients present with is unclear. Antimicrobial therapy with broadly effective agents such as metronidazole has been associated with resolution of diarrhea and even eradication of the intestinal spirochetosis in some patients2.
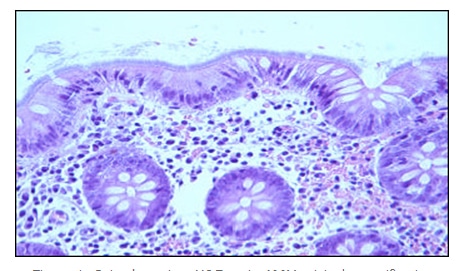
Figure 1: Spirochetosis – H&E stain 400X original magnification
However, metronidazole is effective against a number of gut bacteria thus making a cause/effect statement not possible given current data.
The human colonization rate by spirochetes is variable. Intestinal spirochetosis has been noted in greater frequency in homosexual males yet the medical significance of this finding remains unclear6. The “spread” of human spirochetes is presumed to be via fecal-oral contamination1. That said, it is difficult to speak of fecal-oral contamination and “spread” if in fact the organism is not typically pathogenic and is found in up to 10% of otherwise normal biopsy specimens4,5. The rate of colonization has been shown to vary by geographic location, diet, immune function integrity, and sanitation. Homosexual males may be colonized at a rate of approximately one in three6.
There are typically no endoscopic findings associated with intestinal spirochetosis1. In keeping with the lack of gross findings, the microscopic analysis is equally unimpressive apart from the surface coating by the organisms. There is typically no associated inflammatory response or architectural alteration histologically.
The organisms are seen on the routine hematoxylin and eosin stained sections and can be highlighted with silver based stains as well as Giemsa, periodic acid-Schiff, an acidic alcian blue (pH 2.5) and immunohistochemical stains with spirochete antibodies8. The addition of an immunohistochemical stain using spirochete antibodies is not generally necessary owing to the characteristic appearance on both routine staining and the quicker and less expensive silver-based stain such as Warthin-Starry.
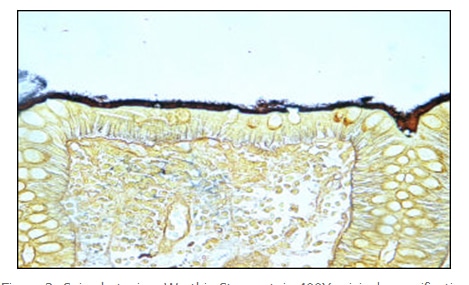
Figure 2: Spirochetosis – Warthin-Starry stain 400X original magnification
Additional studies such as ultrastructural analysis via electron microscopy and Molecular Diagnostics add cost and time and are of little practical utility as speciation, which they are capable of, does not alter therapy9. Culture is not generally successful in common practice as the organisms are fastidious.
Intestinal spirochetosis is an interesting entity; one that is difficult to classify in an appropriate category as placing it under an infectious category of bowel pathology may not even be appropriate. In spite of the reports of relatively high bowel colonization in the study, our large Gastrointestinal Pathology division and others show that it is uncommonly seen at biopsy. Its histologic appearance is unique, striking, and it is readily recognized and demonstrable with simple special stains now if we only knew what it really meant clinically.
I am grateful for the contribution of this interesting case by gastroenterologist Dr. Allen Rubin.
References:
1. Shah R, Stosor V and Badve S. Pathologic quiz case: colon biopsy in a patient with diarrhea – possible etiologic agent. Arch Pathol Lab Med. 2001;125(5):699-700.
2. Pathology of the Gastrointestinal Tract – second edition. Ming SC and Goldman H, eds. Baltimore, MD: Williams and Wilkins. 1998:664.
3. Harland WA and Lee FD. Intestinal spirochetosis. Br Med J. 1967;3:718-719.
4. Henrik-ielsen R, Orholm M, Pederson JO, et al. Colorectal spirochetosis: clinical significance of the infestation. Gastroenterology 1983;85:62-67.
5. Lee FD, Kraszewski A, Gordon J, et al. Intestinal spirochaetosis. Gut. 1971;12:126-133.
6. Ruane PJ, Nakata MM, Reihardt JF, et al. Spirochete-like organisms in the human gastrointestinal tract. Rev Infect Dis 1989;11:184-196.
7. Trivett-Moore NL, Gilbert GL, Law CL, et al.Isolation of serpulina pilosicoli from rectal biopsy specimens showing evidence of intestinal spirochetosis. J Clin Microbiol. 1998;36:261-265.
8. De Brito T, Sandoval MP, Silva AG, et al. Intestinal spirochetosis: first cases reported in Brazil and the use of Immunohistochemistry as an aid in histopathological diagnosis. Rev Inst Med Trop Sao Paulo. 1996;38:45-52.
9. Lee JI, McLaren AJ, Lymbery AJ and Hampson DJ. Human intestinal spirochetes are distinct from Serpulina hyodysenteriae. J Clin Microbiol. 1993;31:16-21.
